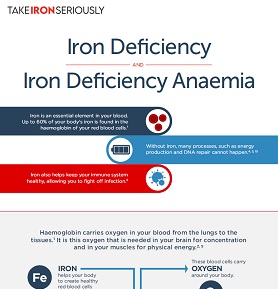
Iron deficiency develops when the amount of iron absorbed by the body does not meet the needs. It can arise either from an inadequate iron in the diet or from a number of different disease conditions that lead to increased iron loss or inadequate usage of iron. It can be considered a continuum, ranging from close to normal iron status, to iron deficiency without anaemia, to, in its most severe form, iron deficiency with anaemia.1,2 Due to this, anaemia is often used as an indicator for iron deficiency. However, also in mild-to-moderate forms of iron deficiency, which have not yet progressed to anaemia, the tissues are lacking iron and are functionally impaired.2 The terms anaemia, iron deficiency and iron deficiency anaemia are sometimes, inappropriately, used interchangeably.2
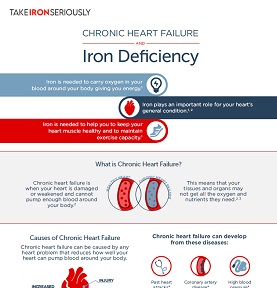
Iron homeostasis can also be affected by chronic disease conditions and inflammation, which can block both the uptake of iron from the gut and the transport of iron. This state eventually leads to anaemia of chronic disease.3
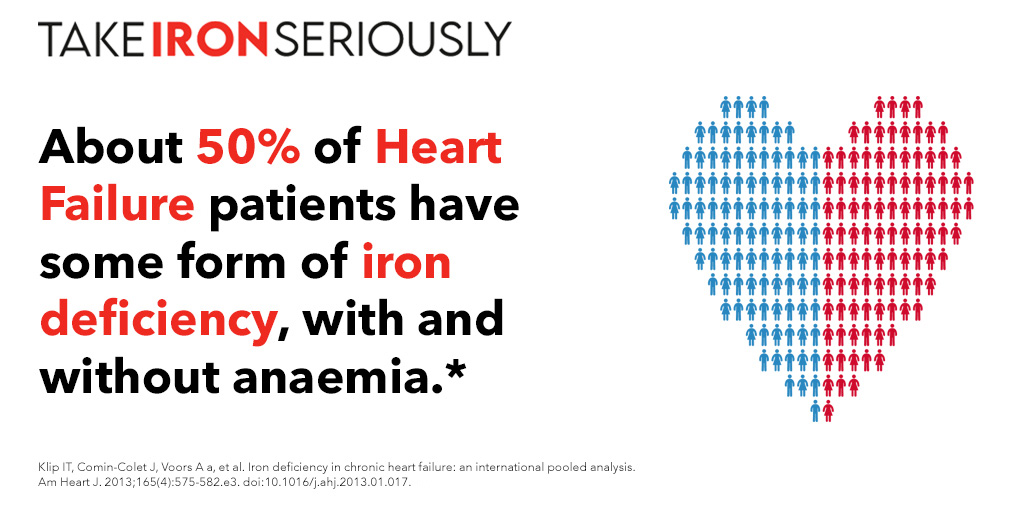
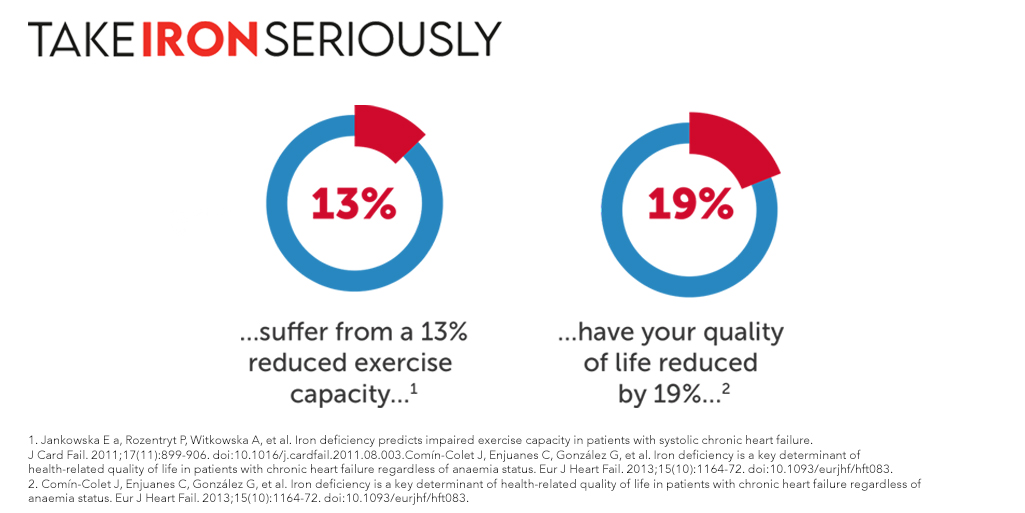
Fatigue is a non-specific symptom, with many different causes. It is recognized as a multidimensional construct involving physical exhaustion, mental tiredness and a lack of energy.4 It is an important healthcare problem, as it is associated with disability comparable to that found in patients with chronic medical conditions5 such as chronic heart failure, chronic obstructive pulmonary disease and rheumatoid arthritis.4,5,6,7,8 Fatigue can have a powerful, adverse effect on quality of life and is considered a phenomenon with social, physiological and psychological dimensions.9

If you are feeling extremely tired or have any of the other symptoms of iron deficiency, it is important to consider whether your diet contains enough iron. Eating more iron-rich foods is a simple way to boost your iron levels and reduce fatigue.
Normally you can get all the iron that your body needs from a healthy, balanced diet.10 However, sometimes you might not eat enough iron-rich foods, even with an otherwise healthy diet. This is especially true for vegetarians and vegans who are more at risk of iron deficiency.11 Iron that comes from plant sources, which is known as non-haem iron, is less well absorbed by your body than iron from animal sources. How well you absorb iron from plant sources is also more affected by other food and drink that you consume around the same time.10 The table below shows examples of iron-rich foods.
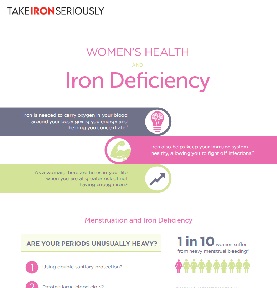
It is also possible that your diet met your body’s iron needs in the past, but that recently your circumstances have changed and now your current iron intake cannot meet the increased demands. This can happen, for example, when you are pregnant or if you have had surgery. You could now think about increasing the iron in your diet so that your iron levels are in balance again.
There is a whole range of iron-rich foods that you can eat more of to help boost your iron levels. Both meat foods containing haem iron12 and vitamin C help with the absorption of non-haem iron. Try to eat iron-rich foods more regularly, think about combining haem and non-haem sources in the same meal (for example red meat and spinach), or add a source of vitamin C (for example, a glass of orange juice) to increase your iron intake.
| Iron Sources (Animal-Based)13 | Iron Sources (Plant-Based)14 |
|---|---|
| Oysters | Soy products |
| Clams | Lentils |
| Red meat e.g. Beef | Beans |
| Liver | Tofu |
| Turkey or chicken giblets | Spinach |
| Fish | Molasses |
| Whole-wheat bread | |
| Peas | |
| Dried fruit (e.g. dried apricots, prunes and raisins) | |
| Iron-enriched cereals and grains (see the packaging for details of iron content)13 |
| Foods that help Iron Absorption | Foods that inhibit Iron Absorption |
|---|---|
| Meat/ sources of haem iron12 | Tea and herbal infusions in general15 |
| Vitamin C e.g. citrus fruits16 | Coffee17 |
| Milk17 | |
| Dairy products17 |
*Calcium, such as that found in milk and dairy products can inhibit iron absorption from both animal-based and plant-based iron sources, unlike the other inhibitors that only affect the absorption of non-haem iron.1
If you are pregnant, or trying to become pregnant, it is important to ask your doctor or midwife about the best iron-rich foods for you to eat, since some foods, such as liver16 or certain types of fish,18 should be avoided during pregnancy.
Similarly, if you have any allergies or dietary restrictions, for example if you have coeliac disease, Inflammatory Bowel Disease (IBD), or have had gastric surgery, speak to your doctor or nutritionist about which foods to eat to increase your iron intake. Your doctor may suggest that you need supplemental sources of iron such as tablets or intravenous iron to get your iron up to within a healthy range. This may also be true if you have iron deficiency anaemia, where diet alone is usually not enough to replace the iron lost.19 Once the iron levels in your body have recovered, eating an iron-rich diet is a good way to keep your iron levels normal.
- Okonko 2011 J Am Coll Cardiol. 2011;58(12):1241-1251. doi:10.1016/j.jacc.2011.04.040
- WHO. Iron Deficiency Anemia. Assessment, Prevention, and Control. A Guide for Programme Managers. 2001.
- Goodnough Transfusion. 2012 Jul;52(7):1584-92. doi: 10.1111/j.1537-2995.2011.03495.x. Epub 2011 Dec 29.
- Radbruch L, Sabatowski R, Elsner F et al. Validation of the German version of the brief fatigue inventory. J Pain Symptom Manage 2003;25:449–458.
- Lewis G, Wessely S. The epidemiology of fatigue: more questions than answers. J Epidemiol Community Health 1992;46:92–97.
- Bergner M, Bobbitt R, Carter W et al. The Sickness Impact Profile: development and final revision of a health status measure. Med Care 1981;19:787–805.
- Bowers S, Cannizzaro K, Gregus J et al. Outcomes in cardiopulmonary physical therapy: sickness impact profile. Cardiopulm Phys Ther J 2009;20:–19.
- Witte KK, Clark AL. Why does chronic heart failure cause breathlessness and fatigue? Prog Cardiovasc Dis 2007;49:366–384.
- Nijrolder I, van der Windt D, de Vries H et al. Diagnoses during follow-up of patients presenting with fatigue in primary care. CMAJ 2009;181:683–687.
- Hurrell R, Egli I. Iron bioavailability and dietary reference values. Am J Clin Nutr. 2010;91:1461-1467. doi:10.3945/ajcn.2010.28674F.Am.
- Killip S, Bennett JM, Chambers MD. Iron deficiency anemia. Am Fam Physician. 2007;75(5):671-8.
- Schümann K, Elsenhans B, Mäurer a. Iron supplementation. J Trace Elem Med Biol. 1998;12(3):129-40. doi:10.1016/S0946-672X(98)80001-1.
- USDA National Nutrient Database for Standard Reference , Release 25 USDA National Nutrient Database for Standard Reference , Release 25. Available at: https://www.ars.usda.gov/SP2UserFiles/Place/12354500/Data/SR25/nutrlist/....
- Penney DS, Miller KG. Nutritional counseling for vegetarians during pregnancy and lactation. J Midwifery Womens Health. 2008;53(1):37-44. doi:10.1016/j.jmwh.2007.07.003.
- Evans EC. The FDA recommendations on fish intake during pregnancy. J Obstet Gynecol Neonatal Nurs. 2002;31(6):715-20.
- Hartmann S, Brørs O, Bock J, et al. Exposure to retinoic acids in non-pregnant women following high vitamin A intake with a liver meal. Int J Vitam Nutr Res. 2005;75(3):187-94.
- World Health Organization. Iron deficiency anaemia. Assessment, prevention and control: A guide for programme managers.; 2001:1-114.
- Evans EC. The FDA recommendations on fish intake during pregnancy. J Obstet Gynecol Neonatal Nurs. 2002;31(6):715-20.
- Michael Alleyne, McDonald K. Horne, MDb, and Jeffery L. Miller M. Individualized treatment for iron deficiency anemia in adults. Am J Med. 2008;121(11):943-948. doi:10.1016/j.amjmed.2008.07.012.Individualized.