Inflammatory bowel disease (or IBD) is a group of chronic idiopathic, relapsing and remitting disorders that cause inflammation of the gastrointestinal tract.1–3Although it was traditionally regarded as a disease of westernised nations, IBD is becoming a global disease at the turn of the 21st century.2 It impacts every aspect of the affected individual's life4 and accounts for substantial costs to the health care system and society.4
Over 3.5 million people affected in the Western world

The prevalence of IBD in the Western world is up to 0.5% of the general population2
- Ng SC, et al. Lancet. 2018;390(10114):2769–2778.
- Kaplan, GG. Nat Rev Gastroenterol Hepatol. 2015;12:720–727.

The types of IBD and risk factors
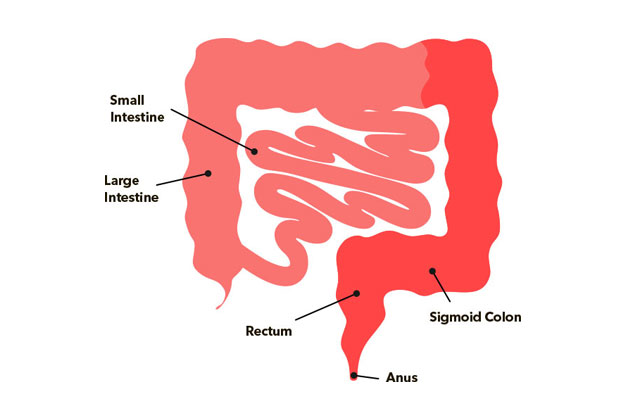
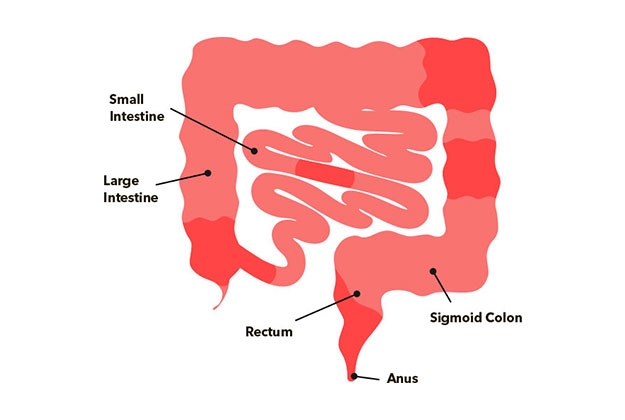
There are two main types of IBD: ulcerative colitis (UC) and Crohn’s disease (CD).5 Ulcerative colitis is a predominantly mucosal disease, its fundamental symptoms is rectal bleeding, and involves the rectum and can affect part of the colon or the entire colon in a continuous pattern.6 In contrast, Crohn’s disease can affect any part of the gastro-intestinal track (from mouth to rectum), although its location more common is the ileum.
Multifactorial Disease
Imbalance of Intestinal Microbiota Causitive & aggravating factors

- Khor B, et al. Nature. 2011;474(7351):307–317.
- Russell R. Postgrad Med J. 2001;77(904):82–88.
- Bjarnason I, et al. Pharmacol Ther. 1994;62(1–2):145–157.
- Mokhtarifar A, et al. Middle East J Dig Dis. 2013;5(2):93–97.
- Ni J, et al. Nat Rev Gastroenterol Hepatol. 2017;14(10):573–584.
- Ananthakrishnan AN, et al. Nat Rev Gastroenterol Hepatol. 2018;15(1):39–49
Although, ulcerative colitis and Crohn’s disease differ in location and depth of inflammation, they share similar symptoms.7 In general, the symptoms depend on the segment of the intestinal tract involved.8 Symptoms related to inflammatory damage in the gastrointestinal tract include diarrhoea (characterised by stools with mucus or blood, nocturnal diarrhoea or incontinence), constipation, pain or rectal bleeding with bowel movement, bowel movement urgency, tenesmus, abdominal cramps and pain, nausea and vomiting.8,9 If you have IBD you are at higher risk of also having iron deficiency and iron deficiency anaemia. Indeed, anaemia is the most common non-intestinal symptom of IBD10.
Ulcerative Colitis1,2
- Rectal pain, with or without diarrhoea
- Bloody diarrhoea
- Rectal bleeding
- Faecal incontinence
- Urgency / tenesmus
- Nocturnal defecation
- Abdominal cramps or pain
- Increased frequency of bowel movements
Crohn’s Disease3
- Abdominal pain often found in the lower right quadrant
- Chronic diarrhoea that can alternate with episodes of constipation
- Rectal bleeding or bloody diarrhoea
- Nausea / vomiting
- Ungaro R, et al. Lancet. 2017;389(10080):1756–1770.
- Magro F, et al. J Crohns Colitis. 2017;11(6):649–670.
- Torres J, et al. Lancet. 2017;389(10080):1741–1755.
Why are you at risk?
If you have IBD of any kind, you are at risk of iron deficiency. Learn more about the risk of IDA.
- WGO Global Guidelines. 2015
- Ng SC et al. Lancet. 2017;390:2769–2778
- Wilhelm SM and Bryan L. Clinical Pharmacist. 2017;Vol 9(3):online. DOI: 10.1211/CP.2017.20202316
- Burisch J et al. J Crohns Colitis. 2013;7(4):322–337
- Kaser A et al. Annu Rev Immunol. 2010;28:573–621
- Guan Q. J Immunol Res. 2019;2019:7247238
- Kim DH and Cheon JH. Immune Network. 2017;17(1):25–40
- WGO Global Guidelines. 2015
- Rowe WA. Inflammatory Bowel Disease: Practice Essentials, Background, Pathophysiology. Medscape. 2017
- Stein J, Hartmann F, Dignass AU. Diagnosis and management of iron deficiency anemia in patients with IBD. Nat Rev Gastroenterol Hepatol. 2010;7(11):599-610. doi:10.1038/nrgastro.2010.151.
If you have IBD of any kind, you are at risk of iron deficiency. Approximately 36%–76% of people with IBD experience iron deficiency anaemia. Learn more about the risk of IDA.
Iron deficiency symptoms can affect many areas of your body. You may experience one or more of these symptoms at the same time. Explore all the signs of iron deficiency.
If you have been diagnosed with IBD you will likely have regular follow-up appointments with your doctor. If you have been feeling fatigued or have any other signs of iron deficiency such as paleness, faintness or a racing heart, you may want to speak to your doctor about your symptoms and iron deficiency. It is useful to think about the information that the doctor might need in order to work out what is causing your symptoms. Your doctor may perform blood tests to check your iron status before suggesting treatment to improve your iron status.
Once your doctor has tested your iron levels they can decide which treatment is best for you. This will depend on the level of iron deficiency you have, and could be advice on how to get more iron in your diet and/or recommendations for medication that you can take to improve your iron levels. More information on the different treatment options and how to get the most iron from your diet can be found by following the link.
If you have IBD of any kind, you are at risk of iron deficiency. Approximately 36%–76% of people with IBD experience iron deficiency anaemia. Learn more about the risk of IDA.
Iron deficiency symptoms can affect many areas of your body. You may experience one or more of these symptoms at the same time. Explore all the signs of iron deficiency.
If you have been diagnosed with IBD you will likely have regular follow-up appointments with your doctor. If you have been feeling fatigued or have any other signs of iron deficiency such as paleness, faintness or a racing heart, you may want to speak to your doctor about your symptoms and iron deficiency. It is useful to think about the information that the doctor might need in order to work out what is causing your symptoms. Your doctor may perform blood tests to check your iron status before suggesting treatment to improve your iron status.
Once your doctor has tested your iron levels they can decide which treatment is best for you. This will depend on the level of iron deficiency you have, and could be advice on how to get more iron in your diet and/or recommendations for medication that you can take to improve your iron levels. More information on the different treatment options and how to get the most iron from your diet can be found by following the link.



